
While the spores multiplythe fungus spreads to the skin of the feet and nails, penetrates through microcracks in the blood and is transported with the bloodstream to all internal organs.
What kind of fungus develops on the toes?

- Toe mycosis is caused by the anthropophilic pathogen Tinea pedis. . .
- Less commonly, the causative agents of the disease are yeast-like molds and fungi of the genus Candida.
- The favorite habitat of the fungus is the folds of the skin between the fingers, where it is warm and humid.
- As the microorganism multiplies, the spores of the microorganism also spread under the toes and thus throughout the foot.
- Primary infection with the fungus occurs in public places: bathrooms, swimming pools, saunas, in the locker rooms of gyms.
- Microorganisms perfectly tolerate low temperatures, excessive dryness of the surface, can persist for a long time in clothes, carpets, shoes and, if the opportunity arises, adhere to the skin of the feet.
- Transmission of the organism often occurs within the family, when using general hygiene items, slippers, manicure tools.
- Getting on the skin, microorganisms are able to remain in a dormant state for a long time. Active growth of spores begins with the onset of favorable conditions, that is, with a decrease in the immunity of an infected person
- If the spores get on the skin of a person suffering from a chronic disease or who does not follow the rules of hygiene, the development of mycosis begins almost immediately.
- It is especially important for patients with chronic diseases to know what the fungus looks like on the fingers, as they are more often infected with the pathogen.

- malfunctions of the endocrine system;
- poor circulation in the limbs, phlebeurysm;
- flat feet,helping to increase the friction of the skin;
- systematic stress;
- periods of hormonal changes in the body: pregnancy, menopause, adolescence;
- inflammation of the lymphatic system;
- postoperative or post-traumaticreduced immunity. . .
The growth of the fungus is favored by sweating of the feet, by shoes in synthetic material and by micro-lesions of the skin.
Favorable conditions for the growth of spores are created with improper nutrition: the abuse of sweets, flour, fatty foods, alcoholic beverages.
In children, toe fungus is rarely diagnosed. The main cause of mycosis in a child is lack of hygiene.
Symptoms and forms of the disease
It is possible to suspect the development of a foot infection in the early stages even before the appearance of visual signs of mycosis.The first sign of infection is peeling and itchy skin.. . .
When microorganisms begin to invade the epidermis, the surface of the fingers becomes covered with small scales and cracks.
An unpleasant smell emanates from the feet. Specific symptoms depend on the form of the disease:
- Deleted.Small cracks and slight peeling form under the fingers and on their surface.
- Squamous-hyperkeratotic.There is severe itching, burning, white crusting on the fingertips.

- Intertriginal.There are swelling, redness of the skin, the formation of moisture between the fingers, peeling of the skin, the formation of deep cracks.
- Dyshidrotic.It occurs with the eruption of small blisters filled with serous fluid. Intense itching, erosion formation at the site of the bursting bubbles, the whole foot becomes inflamed.
IMPORTANT! In the later stages of the disease, the fungus penetrates the surface of the nails and begins to change its color and structure. Nails become covered with colored spots, deform, crumble.
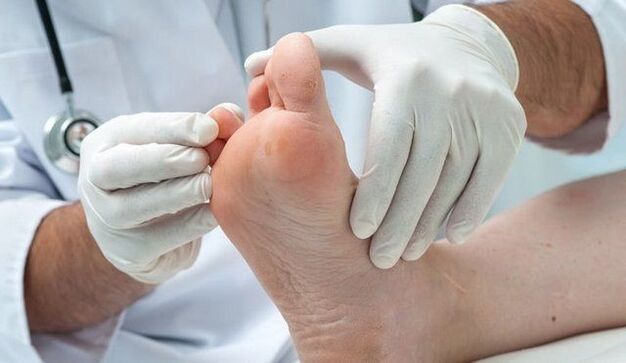
Diagnostics
- When the first clinical signs of infection appear, a doctor should be consulted for a diagnosis.
- Despite the fact that the symptoms of the fungus are clearly visible even in the photo,only a specialist can identify a specific pathogen.
The patient is prescribed laboratory tests:
- Microscopy of skin particles.
- Bacterial culture of scraped and liquid from vesicles.
- DNA research of biomaterials.
- Blood test.
Treatment
- The main activities are -thorough skin hygieneand treatment with topical antifungal drugs.
- In the later stages of the development of a fungal infection, doctors prescribe oral antifungal drugs.
- As accessories to drugs, folk remedies and physiotherapeutic procedures are used.
- It is possible to cure the fungus on the toes by carefully following the recommendations of the doctor, without reducing the time of taking the prescribed drugs.
Drug
Drug treatment involves the use of two groups of drugs:
- External preparations: ointments, creams, gels, sprays.
- Preparations for oral administration.
IMPORTANT! The complex of therapeutic measures also includes a special diet, the intake of immunostimulants and means for restoring the intestinal microflora.
Physiotherapy
Physiotherapy procedures add to drug treatment, accelerate the healing process:
- UV irradiation of the skin. . . The rays penetrate the skin to a depth of 0. 6 mm and kill the fungal spores within it. The duration of the sessions is 15-20 minutes. In the early stages of infection, the use of UV radiation avoids the use of antifungal agents.
- Diathermy,amplipulse therapy, UHF therapy to improve peripheral circulation.
- Laser irradiation of the skin. . . Skin irradiation suppresses inflammation, relieves itching, dries wet areas.
Traditional methods

As accessories to drugs, prepared according to folk recipes, they are quite effective.
According to reviews, effective assistance is provided by the following:
- Baths with soda and salt. . . 1 tablespoon. L. salt and soda are dissolved in 2 liters of water, 10 drops of iodine are added. The feet are immersed in the solution for 15 minutes. The procedure is carried out before applying the antifungal agent.
- Trays with decoction of potato skins. . . The broth is dipped in the broth, which is otsuzhenny at a comfortable temperature, for 20 minutes, then washed. The procedure is carried out daily until the symptoms disappear.
- Trays with poplar bark decoction. . . 100 g of chopped bark is poured into 500 ml of boiling water and insist until it cools. The resulting infusion is added to the bath.
- Garlic ointment. . . 2 large cloves of garlic are crushed into a gruel and mixed with 100 grams of butter. The ointment is applied to the steamed skin for 10-15 minutes a day for a month.
- Decoction applicationsMedicinal herbs. A series of chamomile and violet, 2 tablespoons each, are poured with a liter of boiling water and insisted for 2-3 hours. The infusion-soaked gauze is applied to the inflamed areas for 30 minutes a day.
- Pack with burdock leaf. . . A fresh burdock leaf is removed with a hammer, the legs are wrapped in it, fixed with a bandage, and stockings are put on. The compress is changed 2 times a day. The duration of the course is 21 days.
- Carrot juice applicationsand vinegar. 1 tablespoon. L. carrot juice and 9% vinegar are mixed and applied with a tampon to the inflamed areas.
- Egg and vinegar ointment. . . A raw egg is poured with 100 ml of vinegar essence (70%) and insisted for 7 days. Mix the melted egg with 100 grams of butter, beat. The resulting emulsion is smeared with steamed legs, wrapped in foil and put on socks. The procedure is repeated every day until the fungus has completely healed.
- Compress with ammonia. . . Add 1 tablespoon to 200ml of water. L. ammonia, moisten gauze in a solution, wrap your feet in it and put on socks. The compress is made in the evening and left until the morning. The total number of procedures is 9-10.
Several interesting recipes for the treatment of mushrooms. The use of the methods of traditional medicine necessarily requires the permission of the attending physician.
complications

Spreading in the body and penetrating the bloodstream, the infection affects the internal organs, has a negative effect on the functioning of the whole organism:
- Long-term exposure to fungal toxins causes allergic reactions, exacerbation of bronchial asthma, dermatitis.
- Penetration into the blood disrupts the work of internal organs.
- Deep mycosis causes the progression of diabetes mellitus, and gangrene and bone infections can develop in the background.
Prophylaxis
An organism with a strong immune system is able to resist any infectious disease. Therefore, the main measure to prevent fungal infection is to maintain the body's defenses.
Compliance with hygiene rules will help to avoid infection with fungal spores:
- dailychange of stockings and tights;
- the use of breathable shoes made of natural materials;
- wear special shoes(slippers, slippers) in public places;
- foot skin treatmentspecial protective sprays when visiting swimming pools, baths, beaches;
- do a pedicurein a proven salon,where disinfection of tools is done correctly;
- trying on shoes in a shopin disposable socks. . . To prevent spores from persisting on various surfaces, it is necessary to treat them antiseptically with a 45% vinegar solution.It is advisable to replace wipes and slippers.Treat the rest of the shoes from the inside with a vinegar solution and put them in a plastic bag for 12 hours.
- Boil bedding, stockings, tights, and towels for 10-15 minutes in a solution of soap and soda.

Toe fungus should not be donetherefore, when the first symptoms appear, it is recommended to consult a doctor.
Timely started treatment will allow you to quickly cope with the fungus and avoid complications. It is necessary to treat mycosis until the symptoms are completely eliminated and the skin is restored.
Fungus on the little finger: causes, symptoms (PHOTO) and methods of treatment
Toenail or toenail fungus always begins with the defeat of the outermost toes.
Most often, the big toe is the first to suffer, since its nail is the largest in size, but in some cases the fungus appears first on the little finger.
Such onychomycosis is dangerous for the rapid destruction of the nail plate, which is associated with the small size of the nail on the little finger.
The reasons for the development of the disease

Toenail fungus most often starts with damage to the outer toes
The fungus on the little finger is the result of poor personal hygiene when visiting public places. The fungus spores settle on the skin in public showers and swimming pools. This is due to the fact that the fungus actively reproduces in a humid and warm environment.
Another reason for the development of the disease is profuse sweating and microtraumas of the nail plate. In this case, you can get the disease when you try on shoes, using other people's towels or manicure tools.
Fungus on the little finger of the hand most often occurs as a result of contact with an infected person. A careless handshake can cause the spores to end up under the nail plate.
The main condition for the development of the disease is a decrease in immunity, both general and local. Hyperhidrosis, trauma and damage, circulatory disorders in the extremities - all this leads to a decrease in local immunity and increases the risk of infection.
The peculiarity of the fungal infection of the little finger is the rapid development of the disease. Onychomycosis is caused by fungi that feed on keratin, which is a building material for nails.
The smaller the nail, the faster the pathogenic microflora will destroy it, destroying the keratin, which means that the infection will quickly spread to healthy nails.
If, with a thumb nail injury, the disease progresses slowly and the symptoms increase for months, with onychomycosis of the little finger, the symptoms become evident within a week after the spores of the fungus have entered under the nail.
How to recognize a disease?
The characteristic symptoms of the fungus on the little finger of the nails depend on the exact localization zone. The fungus can affect both the nail and the finger or between the toes. In the first case, the symptoms are as follows:
- yellowing of the nail;
- thickening of the nail plate;
- the appearance of furrows and cracks;
- severe deformation of the nail.
A thick discharge with an unpleasant odor may appear under the nail. The accession of the infection is accompanied by purulent discharge. If left untreated, over time, the nail collapses completely and flakes off the nail bed.
When the skin of the finger is affected, the following symptoms are observed:
- redness of the skin;
- severe itching;
- severe flaking;
- the appearance of an unpleasant odor.
The fungus on the little finger is a serious threat to the rest of healthy fingers, as the spores spread very quickly to healthy skin. In an advanced case, the fungus affects the interdigital spaces, nails and skin of the foot. All this is accompanied by severe itching and an unpleasant smell from the feet.
Diagnostics

If you notice a change in the nail or skin of the little finger, you should visit a dermatologist. The doctor will examine and take the curettage for analysis. In case of skin lesions, flaky scales are sent to the laboratory, which easily separate from the skin.
If the nail plate is affected, the doctor will cut a small piece of the nail and take a swab of exudate under the nail plate. This material is sent to the laboratory for microscopic analysis. Based on the studies carried out, the optimal treatment regimen is selected.
Principle of treatment
To treat the fungus on the little finger, external antifungal agents are used. To get rid of the disease faster, you need:
- monitor personal hygiene;
- regularly take foot baths;
- treat the skin around the affected area with an antiseptic;
- improve immunity.
To avoid the spread of fungal spores on healthy nails, separate manicure tools should be used for the affected finger, disposable files are best. It is imperative to treat the affected area daily with special products, wash the skin thoroughly, carry out an antiseptic treatment and wear only socks and shoes made of natural breathable materials.
Pharmacological treatment
In the treatment of fungal diseases of the feet and with a fungus of the little finger, agents for external use are used, supplementing the treatment with antiseptic baths. In severe cases, the doctor prescribes pills for the fungus.
Only a doctor can choose the exact medicine after the tests. The listed drugs are effective against yeasts and molds. The cream should be applied twice a day on previously washed and dried skin. In this case, the agent must be applied not only to the affected skin, but also to the healthy epidermis around the infected nail.
To avoid the spread of spores to healthy skin areas, antiseptics should also be used. For this purpose, hydrogen peroxide, a solution of potassium permanganate or iodine are used.
Funds in the form of varnish remain on the nail plate for a long time, ensuring effective destruction of pathogenic microflora and preventing further spread of fungal spores.
Nail fungus treatment takes a long time. On average, the course of therapy lasts 9 months. You can stop using drugs only after a healthy nail has grown.
Before applying the varnish, the nails must be steamed, filed and degreased with an alcohol solution or alcohol-containing napkins.
At the initial stage of onychomycosis on the little finger, you can use powerful antifungal creams. The drug is applied after a foot bath and pedicure. In order for the medicine to penetrate deeper into the nail plate, it must be carefully smoothed, eliminating all microfractures.
In severe cases of onychomycosis or if the disease recurs, the doctor may prescribe pills. They have a systemic effect on the whole body, helping to fight pathogenic microflora from the inside.
Nail removal

The nail of the little finger is small in size, almost invisible and grows back rather quickly, so the doctor can recommend a radical treatment method - removal of the nail infected with the fungus. The procedure itself is quick and painless. There are also special kits with uric acid that soften the nail and promote its independent separation from the nail bed.
After removing the nail, a special ointment and bandage are applied to the finger. After 5-7 days, a crust forms under the bandage and can be removed. The nail will start to grow back in about a month. All this time, it is necessary to use antifungal agents to prevent reinfection.
The benefits of nail plate removal minimize the risk of contamination of healthy nails. This allows you to get rid of the fungus in one day, but you will have to wait for the nail to grow back completely. On average, a little finger nail is completely restored in 3-4 months.
Folk remedies
It is recommended to use folk remedies for milder forms of the fungus. They help prevent the spread of spores of pathogenic microflora to healthy fingers, so they perfectly complement drug treatment.
- Lemon juice effectively removes yeast. It can be used for nail infection with Candida fungus, for this it is enough to cover the nail with lemon juice twice a day.
- Mushroom paste will help to defeat the disease. To prepare the product, you need to mix a teaspoon of baking soda with the same amount of water and apply to the nail under a compress. The compress should be held for half an hour, the procedure should be repeated twice a day until the symptoms completely disappear.
- The basis of the folk treatment of the fungus is baths. They can be prepared with iodine, baking soda, salt, hydrogen peroxide, boric acid powder, or herbs. For every liter of water it is necessary to take a tablespoon of the chosen product. Bathing should be done every day before going to bed for 20 minutes.
Folk remedies perfectly prepare the skin and nails for applying ointments from the fungus. As an independent remedy, they are ineffective, so you cannot completely rely on traditional medicine.
How to avoid being infected?
Prevention of fungal infection comes down to personal hygiene. You should always use slippers when visiting public showers and swimming pools, don't use someone else's towels or wear someone else's shoes.
If a person has once contracted a foot fungus, antifungal creams should be used regularly for prevention. For this purpose, it is enough to apply them to the skin 1-2 times a week.
Foot hygiene plays an important role in protecting against fungus. It is necessary to wash your feet daily with antiseptic soap or tar, wear only socks made from natural fabrics and choose comfortable shoes made from breathable materials.
Fungus between the fingers: symptoms (PHOTO), the best ointments and folk remedies for treatment
Of all the types of fungal diseases, foot injuries are the most common.
One type of foot mycosis is a fungus between the toes. The disease causes severe itching and peeling of the skin, which causes severe discomfort. You can get the mushroom in any public place with high humidity.
This type of mycosis occurs in both adults and children.
The reasons for the development of the disease
Fungus between the toes is a type of foot mycosis. The disease is contagious and difficult to cure. The course of therapy can last several months.
Fungus between the toes develops for the following reasons:
- non-compliance with foot hygiene;
- visit public places with high humidity;
- wearing someone else's shoes;
- using someone else's towel.
The easiest way to get an infection is to go to public showers without proper protective equipment. The absence of individual slippers in a shared shower, in a gym locker room or even in a sauna with a moderately high temperature, can cause a fungal infection between the toes, a photo of the symptoms of which will not question the nature peeling of the skin.
The development of fungus between the toes of a child and an adult can be caused by the neglect of personal hygiene. Lack of proper foot care leads to the accumulation of sweat and dirt in the interdigital spaces.
This is a favorable breeding ground for the fungus.
Since some pathogens are always present in the human body, the development of fungal microflora on the skin can occur even without contact with a potential source of infection.
Fungus of the feet and skin between the toes is a highly contagious fungal infection. You can get sick when you try on someone else's shoes, if a person is infected. This is due to the fact that fungal spores settle on the inner surface of the shoe and easily settle on healthy skin.

You can also get sick if a family member is battling a fungal infection. The fact is that the spores of the pathogenic microflora settle on everything that came into contact with the affected skin. Spores persist in the fur of the carpet, on towels and on the surface of the bathroom and shower. The slightest contact with these objects is enough for the spores to penetrate healthy skin.
However, not everyone catches the fungus using someone else's towel or shower. Factors that provoke the development of fungus between the toes:
- decreased immunity, both general and local;
- the presence of damage to the skin of the feet;
- profuse sweating;
- long-term use of antibiotics;
- frequent stress;
- wearing shoes that are too tight;
- diseases that cause poor circulation in the lower limbs.
Long-term drug therapy and frequent stress weaken the body, making it vulnerable to various bacteria and fungi. Wearing tight shoes leads to a violation of local blood circulation, which reduces the immunity of the feet. This creates favorable conditions for the rapid development of pathogenic microflora.
Foot and interdigital fungus is particularly sensitive to people with diabetes, cardiovascular disease and varicose veins of the lower limbs. All these pathologies lead to a deterioration of local metabolic processes and a violation of cellular immunity, thereby increasing the risk of infection with a fungus.
Factors provoking the development of the infection include wearing very tight shoes made of low-quality materials, synthetic socks, and profuse sweating. All this creates a favorable environment for the development of pathogenic microflora. With abundant sweating, the process of increasing the mushroom population is accelerated, as this microflora loves a warm and humid environment.

Folk remedies
Traditional medicine knows how to get rid of the fungus between the toes. For this, it is proposed to use trays and solutions for skin treatment.
- Pour 2 sachets of boric acid into a basin of water and rest your feet for 20 minutes. Apply every other day.
- An effective bath for mycosis: 4 liters of hot water, 2 tablespoons of soda, salt and iodine. Take 15 minutes, then lubricate your feet with medicated ointment.
- You can use applications from a solution of soda with vinegar. To prepare the product, dissolve a teaspoon of soda and vinegar in half a glass of water. Then a cotton swab is moistened in the solution and the skin is carefully treated.
For daily foot hygiene, it is recommended to use tar or laundry soap. They perfectly degrease the skin and have a weak antifungal effect.
Preventing the development of fungus between the toes is thorough foot hygiene. It is important to always bring your own rubber slippers to the swimming pool, gym and sauna. You shouldn't use other people's hygiene items or try on a stranger's shoes, as they may contain fungal spores.
From all that has been said, we can conclude that foot fungus is an extremely dangerous disease. The consequences of the disease can be extremely negative for human health. Do not self-medicate so as not to cause complications.















